Depression, anxiety, post-traumatic stress: protect your brain for tomorrow—starting today
Understanding the link between neuroinflammation and the prevention of neurodegeneration
Key message
During depression, persistent anxiety or post-traumatic stress disorder (PTSD), the body also activates immune alarm pathways: neuroinflammation. When prolonged, this activation can weaken memory, attention and mood. Good news: we can act on it—beyond medication alone.
The brain and the immune system are constantly talking—acting on one influences the other.
What research shows
- Depression: measurable inflammation (e.g., IL-6, IL-17A).
- Anxiety/PTSD: possible inflammatory activation.
- These conditions are associated with a higher risk of cognitive decline.
Why it matters
Whether cause or early warning sign, these conditions indicate a vulnerable terrain. Lowering inflammation supports memory, attention and mood.
Antidepressants & inflammation
Antidepressants are not classical “anti-inflammatories”. Some can modulate inflammatory signals. They fit within a comprehensive strategy: psychotherapy, lifestyle measures and, where appropriate, other approaches targeting inflammation.
Illustrative pathway
- Structured sleep.
- Anti-inflammatory nutrition.
- Appropriate physical activity.
- Stress regulation and vagal tone through distancing techniques.
- Monitoring vascular factors (Aspirin?).
- Dialogue about the role of chronic inflammation.
- Medications (methylene blue, Aspirin, NAC) if indicated, with regular re-evaluation.
Frequently asked questions
Does my antidepressant protect me from dementia?
Not on its own. Some antidepressants can modulate inflammation, but they do not replace a comprehensive plan. That plan includes sleep, nutrition, physical activity, stress skills and medical follow-up.
How do I know if my neuroinflammation is going down?
We can track your symptoms (sleep, concentration, fatigue, mood) and, in some cases, check blood markers. Everyday improvements (more energy, better memory, more stable mood) are already positive signs.
Are blood tests enough?
No. Biological markers tell only part of the story. We combine clinical data (your experience) and biology to adjust the plan.
Can I help myself without medication?
Often yes. Regular sleep, an anti-inflammatory diet, physical activity, stress regulation, social life and time in nature have real protective effects on your brain. If treatment is needed, it complements—rather than replaces—these levers.
Why act early?
Because chronic inflammation acts silently. The earlier we reduce it, the better memory, attention and emotional balance are protected in the long term.
Clinical summary (ultra-brief)
- Depression, anxiety, and PTSD show measurable inflammatory profiles (especially in depression: ↑ IL-6, IL-17A, IL-12, neutrophils/monocytes; ↓ lymphocytes), after excluding inflammatory comorbidities and screening for dementia in older individuals. This supports a plausible “neuroinflammation → neurodegeneration” bridge. (Biomedicines. 2025 Apr 23;13(5):1023. doi: 10.3390/biomedicines13051023) Numerical examples (depression): IL-6 (g≈0.95), neutrophils (g≈3.34), monocytes (g≈3.78), lymphocytes (g≈–1.32). Heterogeneity present but robust effect for IL-6. (Biomedicines. 2025 Apr 23;13(5):1023. doi: 10.3390/biomedicines13051023)
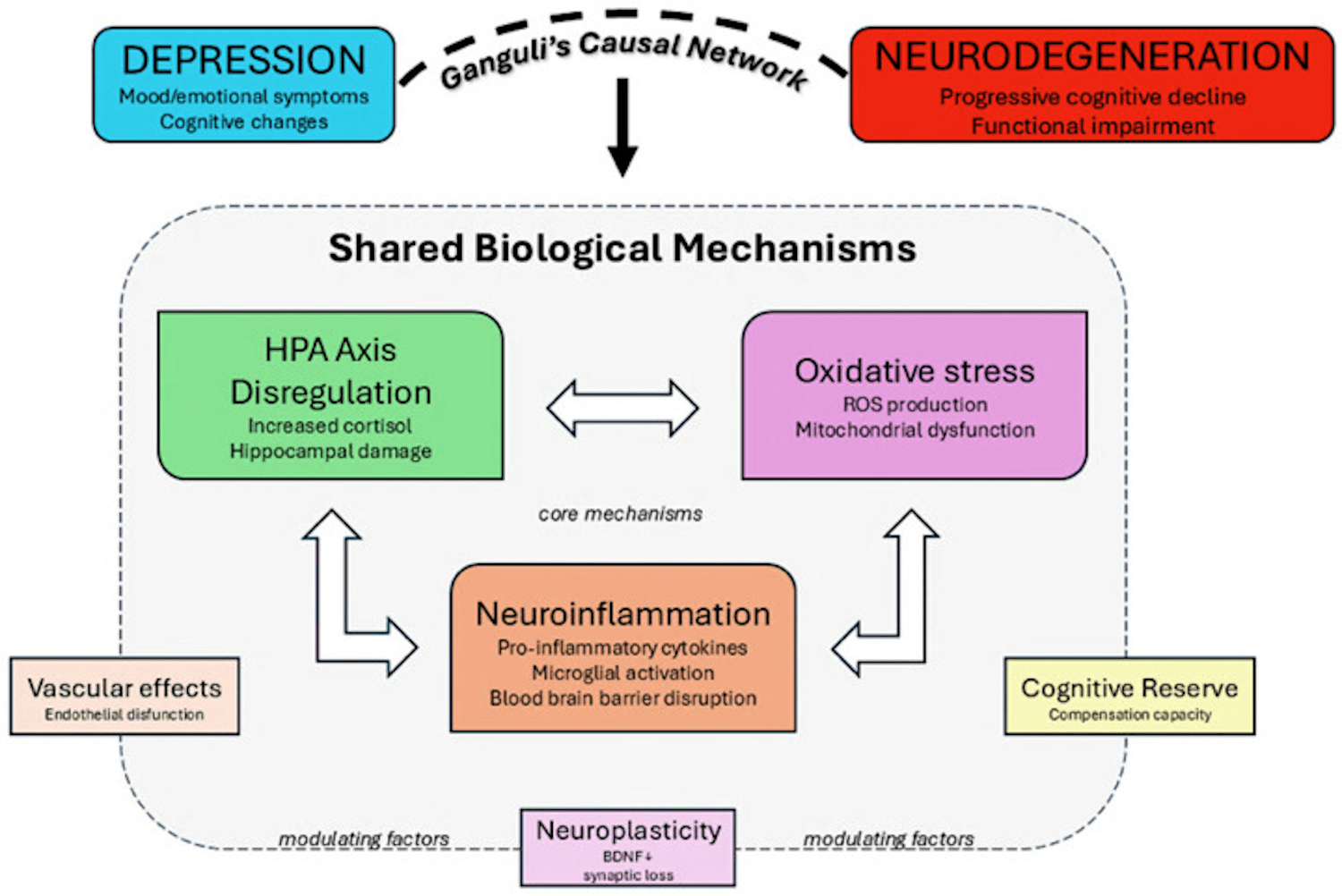
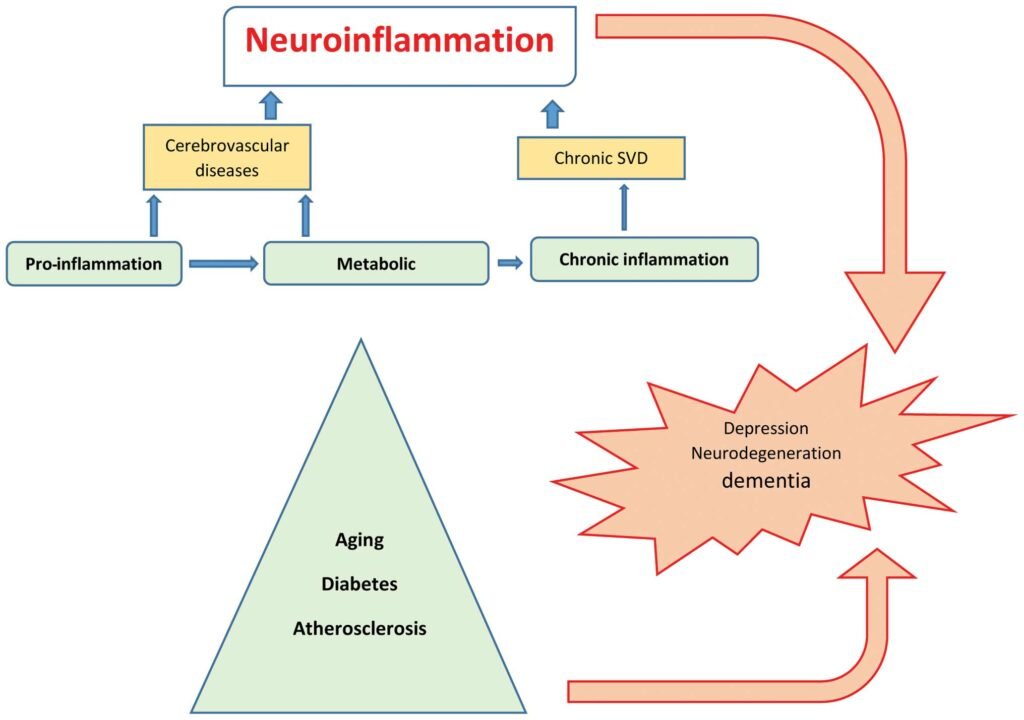
- Link with dementia/PD: recent literature concludes that there is a bidirectional relationship: depression can be a risk factor, prodrome or consequence (depending on age of onset, severity/recurrence, vascular comorbidities/cognitive reserves).. The most coherent mechanistic pathways: neuroinflammation, HPA axis dysregulation, oxidative stress, decreased BDNF, glial/glutamatergic alterations.
- Practical message (even if the prodromal/causal status remains debated): reducing neuroinflammation in anxious/depressed/PTSD patients makes clinical sense, as these disorders are associated with an increased subsequent risk of cognitive decline/dementia and distinct inflammatory signatures.
- Are antidepressants anti-inflammatory? Not “anti-inflammatory” in the classic sense, but several data show immunomodulatory effects (e.g., IL-17/IL-23 variations before/after treatment, effects on Tregs under SSRIs). The effect is neither uniform nor central to their indication, and does not replace a comprehensive anti-inflammatory strategy (lifestyle, sleep, activity, metabolism, stress management, ± anti-inflammatory adjuvants when indicated). (Biomedicines. 2025 Apr 23;13(5):1023. doi: 10.3390/biomedicines13051023)